AeroMedical
Start out with a few of jokes to break the ice.
Why does the FAA not require a medical for glider pilots?
“The Administrator has determined that the environment at the average glider port in the summer, such as Avenal, CA, is such that, if a pilot has a hidden medical problem, that during, or shortly after assembling, pre-flighting, followed by dragging the glider to the take-off area, it is most probable that he or she will die before ever getting into the air. Therefore, it has been determined that a medical is not necessary, since any pilot who survives to get in the air after this type of stress test is deemed most likely fit to survive the rest of the flight itself (within a 5% confidence interval, which is considered by most medical authorities to be a reasonably acceptable or at least a sustainable loss rate).”
The administrator may not know that we have golf carts now to tow the gliders, as the rule was written quite a few years ago. But suspect the basic premise is still true.
In a way, this is not really a joke, because a lot of people who have been grounded from power flying due to potentially serious medical problems such as heart attacks, and even strokes, diabetics on insulin etc, etc. actively seek out glider flying as an alternative. However, their risk is not necessarily less flying gliders and the environment is really often much harsher in gliding than in power flying.
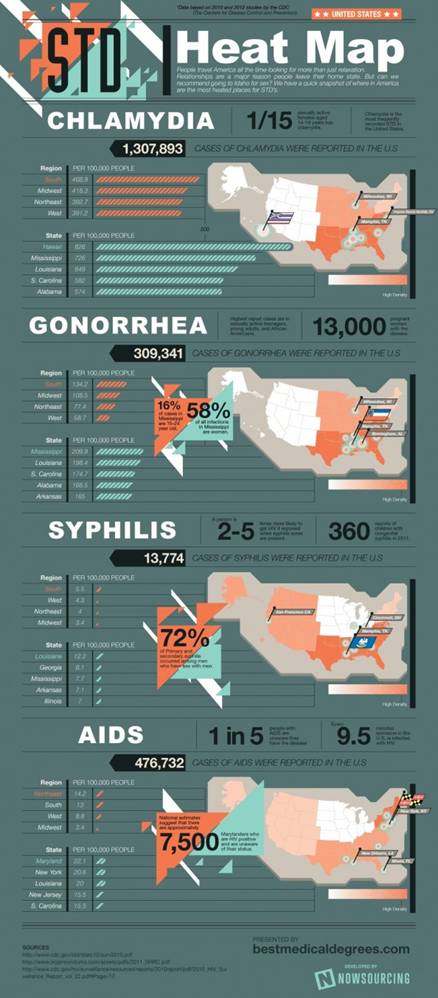
STD Hotspot Map for landouts.
Treatment center Map in case above fails to prevent aquisition.
Circ. Joke.
Were any of you born between the years 1971 and 1978,
inclusive, in either
Self Assesment
CFR 62.23(b)
(b) Operations not requiring a medical certificate. A
person is not required to hold a medical certificate—
(1) When exercising the privileges of a student pilot
certificate while seeking—
(i) A sport pilot certificate with
glider or balloon privileges; or
(ii) A pilot certificate with a glider category rating or
balloon class rating;
(2) When exercising the privileges of a sport pilot
certificate with privileges in a glider or balloon;
(3) When exercising the privileges of a pilot certificate
with a glider category rating or balloon class rating in a glider or a balloon,
as appropriate;
(4) When exercising the privileges of a flight instructor
certificate with—
(i) A sport pilot rating in a
glider or balloon; or
(ii) A glider category rating;
CFR 62.53(b)
(b)
Operations that do not require a medical certificate. For operations
provided for in § 61.23(b) of this part, a person shall not act as pilot
in command, or in any other capacity as a required pilot flight crewmember,
while that person knows or has reason to know of any medical condition that
would make the person unable to operate the aircraft in a safe manner.
Glider pilots not required to have a medical, but are still required to ground themselves when they have a known condition that would render them unsafe to fly. Big responsibility when you think about it. What guidance can we look to in making these decisions?
Before flight pilots should do a self medical assessment. Overlaps some between
Strictly Medical and the Psychological
Examples of some people who misjudged their fitness to fly:
RJ – did not take anyone else with him. Operating with an unsuspecting passenger is a
lot different in most people’s minds to flying by yourself
in a remote unpopulated area, although this is not the way the
IMSAFE Mnemonic
Illness
Medication
Stress – some is good but too much can be overwhelming.
Alcohol
Fatigue
Eating
Five Hazardous Attitudes
“The Loose Cannon”
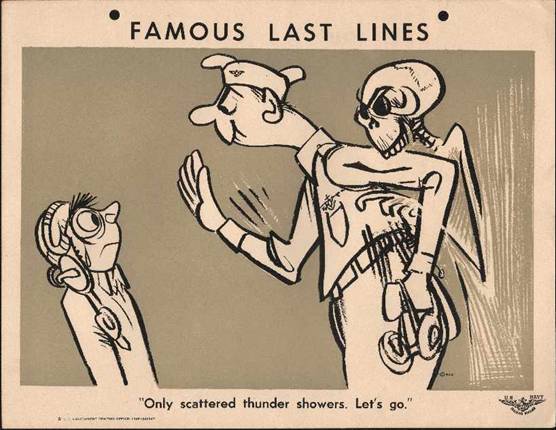
The military during WWII had a huge pilot training program with a very big budget. They drafted or got volunteer service from some of the best and brightest of the era on their training materials. One of the outstanding ones was Robert C. Osborn, the creator
of “Dilbert”.
“Dilbert” – US Navy training manual cartoon character. Exhibited all 5 hazardous attitudes and many more. These illustrations were created by Robert C. Osborn while he was commissioned as a Navy officer during WWII. This guy was REALLY good. The cartoon format really helped make some of the lessons sink in better. Too bad the FAA doesn’t have somebody like him available for their training handbook instead of the current batch of dry psychology stuff.
I will include the five “Hazardous Attitudes” in this area even though they are more psychological than strictly medical.
Macho – “I can do it! I’ll show them!” Antidote - Taking chances is foolish
Anti-Authority - “Don’t tell me!” Antidote - Follow the rules, they are usually right, i.e. “written in blood”.
Invulnerability – “It can’t happen to me!” Antidote – It CAN happen to me!
Impulsivity- “Do it quickly” Antidote- Not so fast. Think first.
Resignation- “What’s the use?” Antidote – I’m not helpless. I can make a difference.
Hypoxia
Occurs when the tissues of the body do not receive enough oxygen. Symptoms vary with the individual. Causes are insufficient supply, inadequate transportation, inability of tissues to take up the oxygen. Symptoms are subtle and often the first symptom is a false sense of euphoria or well being. Later symptoms may be headache, drowsiness, light headedness, decreased reaction time, impaired judgement, tingling, numbness, visual loss or disturbances, blue fingernails and lips, weak muscles. For purposes of discussion, there are four kinds of hypoxia:
Hypoxic Hypoxia
The percentage of oxygen stays the same with increased altitude, but the partial pressure or the number of oxygen molecules available to the body and tissues is reduced with high altitude.
Hypemic Hypoxia
Reduced ability of the blood to deliver the oxygen to the tissues. Anemia, CO poisoning and other medical factors. Donating blood can affect you for a time. Usually not on the ground but becomes more noticeable at high altitude.
Stagnant Hypoxia
Reduced circulation of the blood. Can be due to cold, increased G loads. Constricted arteries. Venous poolling due to prolonged immobilization.
Histotoxic Hypoxia
Delivery of Oxygen OK, but cells not able to take it up. Alcohol, drugs, poisoning.
Sec. 91.211 — Supplemental oxygen.
(a) General. No person may operate a civil aircraft of
(1) At cabin pressure altitudes above 12,500 feet (MSL) up
to and including 14,000 feet (MSL) unless the required minimum flight crew is
provided with and uses supplemental oxygen for that part of the flight at those
altitudes that is of more than 30 minutes duration;
(2) At cabin pressure altitudes above 14,000 feet (MSL)
unless the required minimum flight crew is provided with and uses supplemental
oxygen during the entire flight time at those altitudes; and
(3) At cabin pressure altitudes above 15,000 feet (MSL)
unless each occupant of the aircraft is provided with supplemental oxygen.
|
FL 150 |
30 min or more |
4,572 m |
15,000 |
|
FL 180 |
20 to 30 min |
5,486 m |
18,000 |
|
FL 220 |
5-10 min |
6,705 m |
22,000 |
|
FL 250 |
3 to 6 min |
7,620 m |
25,000 |
|
FL 280 |
2.5 to 3 mins |
8,534 m |
28,000 |
|
FL 300 |
1 to 3 mins |
9,144 m |
30,000 |
|
FL 350 |
30 sec to 60 sec |
10,668 m |
35,000 |
|
FL 400 |
15 to 20 sec |
12,192 m |
40,000 |
|
FL 430 |
9 to 15 sec |
13,106 m |
43,000 |
|
FL 500 and above |
6 to 9 sec |
15,240 m |
50,000 |
This can be reduced by Old Age, SMOKING, rapid
decompression, any pulmonary disease.
Altitude Chamber Flights can be arranged to experience
hypoxia first hand.
FAA Civil Aerospace Medical Institute and many military
bases can arrange for groups to have chamber sessions.
405-954-6212
Hyperventilation
Often triggered by fear or panic. Sometimes by trying to blow up a balloon, air mattress etc.
Rapid breathing rate causes CO2 to be disproportionately “blown off’ when expiring and thus the pCO2 of the blood decreases below normal. This results in reduced respiratory drive, and subsequently can result in hypoxia, since the brain’s respiratory center primarily responds to carbon dioxide to stimulate respiratory rate rather than oxygen. It also can rapidly result in an increased, or more alkaline, pH in the blood, which accounts for many of the symptoms - light headedness, dizziness, tingling of fingers and toes, and muscle spasms. Solution is to slow respiratory rate. It may help to hold a paper bag loosely (not tightly sealed) near the face. Singing may help. Relaxing and calming down, “talking the person down” helps, if possible. But these measures may be difficult in a panic situation. Symptoms will reverse fairly quickly, but not immediately when proper measures are taken.
Middle Ear and Sinus Problems
Paranasal sinuses, Frontal, maxillary, sphenoid, ethmoid
Middle Ear Cavity, Mastoid air cells
All closed hollow air spaces that communicate with the outside air via small narrow
Passages into the nose and pharynx. If these passages are blocked due to conditions such as colds or allergies, you may not be able to equalize the air pressure between the sinuses and/or middle ear cavity and the outside air. This can result in extreme pain. Often, you will be able to ascend without too much trouble. But when you try to descend, you will have more trouble equalizing the pressure. The symptoms may be sudden severe pain in the areas affected. If you are lucky, you may be able to do a “Valsalva” maneuver to force air into the sinuses and middle ear cavities by holding your nose and blowing gently. But it may not work if the blockage is really bad. In this case, it can take a long time (days, weeks or even longer) to improve, and may result in damage to the eardrums and possible sinus problems such as infections etc., besides it’s REALLY painful! Many OTC cold and allergy meds contain drugs that cause drowsiness, such as antihistamines. Decongestants may help but can exacerbate HTN and may be very irritating and cause a “rebound” congestion if used more than a very short time .
Spatial Disorientation
Lack of orientation with regards to position in space and to other objects. Orientation is maintained through the body’s sensory organs in three areas: visual, vetibular, and postural. The eyes maintain visual orientation; the motion sensing system in the inner ear maintains vestibular orientation; and the nerves in the skin, joints and muscles of the body maintain postural orientation.
During flight in visual meteorological conditions “VMC” or “VFR”, the eyes are the major orientation source and usually prevail over false sensations from other sensory systems. When these visual cues are taken away, as they are in instrument meteorological conditions “IMC” or “IFR”, false sensations can cause the pilot to quickly become disoriented.
The vestibular system in the inner ear allows you to sense movement and determine your orientation in the surrounding environment. In both the left and right inner ear, three semi-circular canals are positioned at approximate right angles to each other. Each canal is filled with fluid and has a section full of fine hairs. Acceleration of the inner ear in any direction causes the tiny hairs to deflect, which in turn stimulates nerve impulses, sending messages to the brain. The vestibular nerve transmits the impulses from the utricle, saccule, and the semicircular canals to the brain to interpret motion.
The postural system sends signals from the skin, joints, and muscles to the brain that are interpreted in relation to the Earth’s gravitational pull. These signals determine posture. Inputs from each movement update update the body’s position to the brain on a constant basis. “Seat of the pants” flying is largely dependent upon these signals. Used in conjunction with visual and vestibular clues, these sensations can be fairly reliable. However, because of the forces acting on the body in certain flight situations, many false sensations can occur due to acceleration forces overpowering gravity.
Under normal flight conditions, when you have reference to the horizon and ground, these sensitive hairs allow you to identify the pitch, roll, and yaw movement of the glider. When you become disoriented and lose visual reference to the horizon and ground, the sensory system in your inner ear is no longer reliable. Lacking visual reference to the ground, your vestibular system mayh lead you to believe you are in level flight, when, in reality, you are in a turn. As the airspeed increases, you may experience a postural sensation of a level dive and pull back on the stick. This increased back-pressure on the control stick tightens the turn and creates ever-increasing g-loads. If recovery is not initiated, a steep spiral will develop. This is sometimes called the “Graveyard Spiral”, because if the pilot fails to recognize that the aircraft is in a spiral and fails to return the aircraft to wings-level flight, the aircraft will eventually strike the ground. If the horizon becomes visible again, you will have an opportunity to return the glider to straight-and-level flight. Continued visual contact with the horizon will allow you to maintain straight-and-level flight. However, if you lose contact with the horizon again, your inner ear may fool you into thinking you have started a bank in the other direction, causing the graveyard siral to begin all over again.
For glider pilots, prevention is the best remedy for spatial disorientation. If the glider you are flying is not equipped for instrument flight, and you do not have many hours of training in controlling the glider by reference to instruments, you should avoid flight in reduced visibility or at night when the horizon is not visible. You can reduce your susceptibility to disorienting illusions throught training and swareness and learning to rely totally on your flight instruments.
Motion Sickness
Motion sickness, or airsickness is caused by the brain receiving conflicting messages about the state of the body. You may experience motion sickness during initial flights, but it generally goes away within the first 10 lessons. Anxiety and stress, which you may feel as you begin flight training, can contribute to mition sickness. Symptoms of motion sickness include general discomfort, nausea, dizziness, paleness, sweating, and vomiting.
It is important to remember that experiencing air sickness is no reflection on your ability as a pilot. Let your flight instructor know if you are prone to motion sickness, since there are techniques that can be used to over come this problem. For example, you may want to avoid lessons in turbulent conditions until you are more comfortable in the glider, or start with shorter flights and graduate to longer instruction periods. If you experience symptoms of motion sickness during a lesson, you can alleviate some of the discomfort by opening fresh air vents or by focusing on objects outside the glider. Although medication like Dramamine can prevent airsickness in passengers, it is not recommended while you are flying since it can cause drowsiness.
Ginger may help some people. Not flying on an empty stomach may help. Some people feel that a small drink of a carbonated beverage may help, other do not.
Carbon Monoxide Poisoning
One factor that can affect your vision and consciousness in flight and poses a danger to self-launch glider pilots is carbon monoxide poisoning. Since carbon monoxide attaches itself to the hemoglobin about 200 times more easily than does oxygen, carbon monoxide (CO) prevents the hemoglobin from carrying oxygen to the cells. It can take up to 48 hours for the body to dispose of carbon monoxide. If the poisoning is severe enough, it can result in death. CO, produced by all internal combustion engines, is colorless and odorless. Aircraft heather vents and defrost vents may provide CO a passageway into the cabin, particularly if the engine exhaust system is leaky or damaged. If you detect a stron odor of exhaust fumes, you can assume that carbon monoxide is present. However, carbon monoxide may be present in dangerous amounts even if you cannot detect exhaust odor. Disposable, inexpensive carbon monoxide detectors are widely available. In the presence of CO, these detectors change color to alert you to the presence of CO. Some effects of CO poisoning include headache, blurred vision, dizziness, drowsiness, and/or loss of muscle power. Anytime you smell exhaust odor, or any time you experience these symptoms, immediate corrective actions should be taken. These include turning off the heater, opening fresh air vents, windows and using supplemental oxygen, if available.
Stress
Physical – temperature, vibration, noise, extremes of humidity, lack of oxygen
Physiological – Illness, fatigue, lack of physical fitness, lack of sleep, missed meals, low blood sugar
Psychological - Social and Emotional Problems - divorce, death in family, sick child, demotion at work, interpersonal conflicts.
Acute Stress – flight or fight response. Can turn chronic.
Chronic Stress – intolerable burden exceeding the ability of the person to cope, causes performance to fall sharply. Lonliness, financial worries, relationship or work problems.
You should not fly if you are under this type of stress as performance can fall off dramatically, affecting safety.
Fatigue
Can be sleep loss, exercise or physical work.
Acute and chronic.
Physical fatigue
Hypoxia, Mental stress
Rest, proper diet very important to optimal functioning.
Chronic fatigue can lead to certain glandular changes such as cortisol etc that may take longer to correct than just a good night’s rest
Dehydration and Heatstroke
You must drink lots of water. Sports drinks – generally OK, but if you eat a good reasonable meal for breakfast and at least a snack at lunch time and are not vomiting etc,
You will get enough electrolytes from the food. Coffee not too good because it has a diuretic effect.
Wear light colored porous clothing. Always wear a hat and eye protection. Glove are good too, as you get a lot of sun on your hands flying a glider.
Glider Pilot Fashion Show. Good garb for protection in the gliding environment:

Not so good, but at least the sun was going down!

Thirst not a good sign of dehydration because it is a relatively late symptom. You already may be significantly dehydrated i.e. 3% or even 5% by the time you actually feel thirsty and it can be hard to catch up. It is better to prevent it, and anticipate it and hydrate up.
When you get very high and it gets cold, like under clouds at altitude, your body will constrict blood vessels in the extremities to conserve heat. This causes the vascular system to feel that it is “overloaded” and needs to get rid of some of the excess water, so you will soon have to pee. You will be OK while you’re up there and it’s cold, but when you descend and it gets real hot again near the ground, you will suddenly be way behind on your fluids and need to re-hydrate again. Anticipate this need, and have liquid available to accomplish it as soon as you start descending.
For any planned flight over an hour or so it is very important to plan on a means of being able to pee. Do not let yourself dehydrate to avoid having to pee while in flight. This is a commonly done thing and is dangerous.
Heat exhaustion - dehydration, weakness, fainting.
Heat stroke. – very
serious emergency. Body loses ability to control temperature which can go up to
fatal levels. Every year people die in
the
Alcohol
We all know it is a drug and affects our judgement and performance. In larger amounts it is a literal poison and can kill you directly through toxicity with depression of the brain and respiration, or indirectly through choking, aspiration etc. Altitude magnifies the effects of alcohol.
CFRs – 0.04 % is the maximum permissible level in the blood. Also 8 hours must pass between drinking any alcohol and piloting an aircraft regardless of the blood level.
Drugs
Both OTC and prescribed can be bad.
Tranquilizers
Xanax, Valium, Librium,
Sedatives
Strong pain relievers
Percodan,
Demerol, Vicodin,
Cough suppressants
Phenergan with codeine, hycodan etc.
Often contain alcohol, antihistamines or phenothiazines and narcotics like codeine, or hydrocodone .
Stimulants
Phentermine
Decongestants
Sudafed, Nasal sprays like Dristan, Afrin, Neosynephrine
Often act like stimulants.
Antihistamines
Antacids
Pepcid, Tagamet – May be OK but require approval for Power flying by an AME.
If you have actually had a bleeding ulcer, you may be grounded without a “Special Issuance”.
Blood pressure medications
Centrally acting ones cause drowsiness. Not used as much these days.
Reserpine, Aldomet, Clonidine
Beta Blockers can be bad combined with insulin – not allowed by the FAA
Muscle Relaxants
Soma, Flexeril, Robaxin, Skelaxin
Antidiarrheals
Lomotil
Anti-emetics Anti-nausea
Anti-Motion Sickness Drugs
Antihistamines – Dramamine, Meclizine
Phenothiazines – phenergan, compazine
Scopolomine – Transderm Scop Patches – can cause severe hallucinations affect your ability to withstand heat.
Illegal Drugs
Cannibis
Narcotics
Cocaine
Usually OK
Tylenol / acetaminophen
Asprin
Ibuprofen – Advil - Motrin
Aleve – Naprosyn – Naproxyn
Local anesthetics usually wear off in a few hours but you may not be in shape to fly if you are having pain or are uncomfortable from the procedure.
The use of a psychotropic drug is disqualifying for aeromedical certification purposes. This includes all
sedatives, tranquilizers, antipsychotic drugs, antidepressant drugs (including SSRI's – see
exceptions), analeptics, anxiolytics, and
hallucinogens. The Examiner should defer issuance and forward the medical
records to the AMCD.
Guide for Aviation Medical Examiners
Decision Considerations - Aerospace Medical Dispositions
Item 47. Psychiatric Conditions - Psychiatric Conditions Table of Medical
Dispositions
|
Disease/Condition |
Class |
Evaluation Data |
Disposition |
|
Adjustment Disorders |
All |
Submit all pertinent medical information and clinical status report |
If stable, resolved, no associated disturbance of thought,
no recurrent episodes, and psychotropic medication(s) used for less than 6
months and discontinued for at least 3 months - Issue |
|
Attention Deficit Disorder |
All |
Submit all pertinent medical information and clinical status report to include documenting the period of use, name and dosage of any medication(s) and side-effects |
Requires FAA Decision |
|
Bipolar Disorder |
All |
Requires FAA Decision |
|
|
Bereavement; |
All |
Submit all pertinent medical information and clinical status report |
If stable, resolved, no associated disturbance of thought,
no recurrent episodes, and; |
|
Depression requiring the use of antidepressant medications |
All |
Submit all pertinent medical information and clinical
status report. |
Requires FAA Decision |
|
Personality Disorders |
All |
Requires FAA Decision |
|
|
Psychosis |
All |
Requires FAA Decision |
|
|
Pyschotropic medications for Smoking Cessation |
All |
Document period of use, name and dosage of |
If medication(s) discontinued for at least 30 days and w/o
side-effects - Issue |
|
Substance Abuse |
All |
Requires FAA Decision |
|
|
Substance Dependence |
All |
Requires FAA Decision |
|
|
Suicide Attempt |
All |
Submit all pertinent medical information required |
Requires FAA Decision |
Guide for Aviation Medical Examiners
Pharmaceuticals (Therapeutic Medications)
Diabetes Mellitus - Insulin Treated
- Code of Federal Regulations
- First-Class Airman Medical Certificate: 67.113(a)(b)(c)
- Second-Class Airman Medical Certificate: 67.213(a)(b)(c)
- Third-Class Airman Medical Certificate: 67.313(a)(b)(c)
- Medical History: Item
18.k., Diabetes.
The applicant should describe the condition to include, symptoms and treatment. Comment on the presence or absence of hyperglycemic and/or hypoglycemic episodes. A medical history or clinical diagnosis of diabetes mellitus requiring insulin or other hypoglycemic drugs for control are disqualifying. The Examiner can help expedite the FAA review by assisting the applicant in gathering medical records and submitting a current specialty report. - Aeromedical
Decision Considerations: See Item
48, General Systemic Aerospace Medical Disposition table. The FAA has
established a policy that permits the special issuance medical
certification of insulin treated applicants for third class
medical certification only. Consideration will be given only to
those individuals who have been clinically stable on their current
treatment regimen for a period of 6-months or more.
- Protocol: See Insulin-Treated Diabetes Mellitus - Type I or Type II, Protocol
- Pharmaceutical Considerations:
- Insulin pumps are an acceptable form of treatment.
- Combination of insulin with beta-bockers is not permitted.
- Combination of insulin with other anti-diabetes medication (s): not all combinations of DM medications are allowed by the FAA, even if each medication within the combination is acceptable as monotherapy. Contact Regional Flight Surgeon’s office or AMCD
Scuba Diving
Danger of nitrogen narcosis or the Bends
Allow 12 hours between non-decompression diving and flying.
Allow 24 hours between decompression requiring diving and any flying.